The Rise in STIs Post-COVID
By Dr Sudha Pottumarthy-Boddu, Dr Stella Pendle and Dr Linda Dreyer
Published
March 2024
The Changing Landscape of STIs: Test, detect and treat are the keys to control
By Dr Sudha Pottumarthy-Boddu
The impact of the COVID-19 pandemic extends beyond economic and social disruption, with a direct and indirect impact on the health of individuals worldwide. The low coverage for prevention, testing, and treatment services for STIs during the pandemic has led to a resurgence of STIs globally. Over 1 million new sexually transmitted infections are acquired worldwide every day, with the majority being asymptomatic. The World Health Organization (WHO) in 2020 estimated 374 million new infections with one of the four common STIs: chlamydia (129 million), gonorrhoea (82 million), syphilis (7.1 million), and trichomoniasis (156 million). The incidence of genital infection with herpes simplex virus (HSV) among 15 to 49-year-olds is estimated to be over 500 million.1
Post-pandemic resurgence: STI trends in Australia
Trends in key bacterial notifiable STIs, as noted in the National Communicable Disease Surveillance Dashboard of Australia, mimic the global trends2. Three years, 2020 to 2022, saw a drop in notifications compared to 2019, reflecting the impact of the pandemic (see Table 1). However, 2023 saw a resurgence of STIs, with notifications significantly higher than in 2019, especially for syphilis < 2 years duration (8.6 % increase), gonococcal infection (16% increase), and congenital syphilis (400% increase; 4 each in VIC, WA, and NSW and 5 in QLD) (Table 1).2
Table 1. Trends in Key Notifiable STIs in Australia – 2019 to 2023
| STI | 2019 | 2020 | 2021 | 2022 | 2023 |
|---|---|---|---|---|---|
| Chlamydial infection | 107,396 | 91,449 | 87,367 | 94,365 | 109,894 |
| Gonococcal infection | 34,745 | 29,801 | 26,599 | 33,148 | 40,404 |
| Syphilis < 2 years of duration | 5,915 | 5,361 | 5,775 | 6,180 | 6,451 |
| Syphilis > 2 years or unspecified duration | 2,609 | 2,192 | 2,186 | 2,623 | 2,795 |
| Congenital Syphilis | 4 | 17 | 15 | 15 | 20 |
Rising congenital syphilis cases in the US
Addressing missed opportunities, the CDC (Centers for Disease Control) reported a 755% increase in congenital syphilis cases in the United States from 2012 to 2021 (335 versus 2,865 respectively), with 3,761 cases reported in 2022 (231 stillbirths and 51 infant deaths).3 Lack of timely testing and adequate treatment during pregnancy contributed to almost 90% of these preventable cases.
New infections and antibiotic resistance
In addition to the ongoing impact of recognised STIs, other concerning facts include:
- New infections that can be acquired by sexual contact have emerged and are leading to outbreaks in some instances. These include mpox, Shigella sonnei, Neisseria meningitidis, Ebola and Zika, along with the re-emergence of neglected STIs like lymphogranuloma venerum (LGV).1
- Emergence and spread of multi-drug-resistant gonorrhoea: Resistance of N.gonorrhoeae to the available antimicrobial options continues to evolve, with recognition of high levels of resistance to ciprofloxacin, increasing resistance to azithromycin, and resistance or decreased susceptibility to cefixime and ceftriaxone.4
STI co-infections: Implications and recommendations
Accurate rates of STI co-infections are often difficult to discern as the infections are notified separately. However, it is well recognised that persons at risk of STI acquisition are also at risk of co-infection with more than one STI. Co-infection of Chlamydia trachomatis in individuals diagnosed with Neisseria gonorrhoeae is well recognised. However, there is paucity of data on the co-infection of chlamydia and gonorrhoea among persons with early syphilis.
A recent study from the University of Birmingham in Alabama reported that of the 865 adults enrolled for a controlled trial for treatment of early syphilis, 234 (27%) adults had also had documented STI co-infection, of whom 29% had N. gonorrhoeae, 22% had C.trachomatis, and 23% had both. Multisite STI screening for multiple pathogens is recommended for sexually active adults at risk to identify both symptomatic and asymptomatic infections.
Neisseria meningitidis: A newly emerging sexually transmitted infection
By Dr Stella Pendle
N. meningitidis and N. gonorrhoeae: Causes and risks
Neisseria meningitidis (NM) is typically found as a commensal in the upper respiratory tract of humans and is a leading cause of sepsis. It has the unique ability to cause outbreaks of invasive meningococcal disease, which can be fatal. Neisseria gonorrhoeae (NG) traditionally causes gonorrhoea, a sexually transmitted infection involving the genitals, rectum, and throat. These species usually occupy distinct niches but may cause reciprocal diseases. NM may also occasionally be found in the genital tract as a commensal. It has long been recognised that urethral NM infections could be spread by oral sex and were more common in men who have sex with men.6
Urogenital and anogenital infections due to N. meningitidis
In recent years, there have been increasing reports worldwide of urogenital and anogenital infections attributed to NM. These may mimic the symptoms of gonorrhoea, causing urethritis, proctitis, cervicitis, and pelvic inflammatory disease, which is indistinguishable from gonorrhoea. In addition, meningococcal urethritis has been documented in long-term monogamous relationships in which the partner has no disease.7,8
Changing patterns of meningococcal urethritis
At the beginning of the 21st century, meningococcal urethritis was considered to be a rare condition, found almost entirely in MSM and transmitted by oral sex. More recently, clusters of meningococcal urethritis were identified predominantly in heterosexual men, mainly in the 20 to 30 years age group. Symptoms included urethral discharge (>90%) and dysuria, with symptoms ranging from 2 to 7 days. Almost all men with meningococcal urethritis reported oral sex encounters. However, genitalgenital and ano-genital infection can also occur. Like N. gonorrhoeae, N. meningitidis can also cause cervicitis, vulvovaginitis, pelvic inflammatory disease, salpingitis, endometritis, and proctitis. Neonatal conjunctivitis and pre-term birth have also been reported. Cases of invasive meningococcal disease (IMD) secondary to infection and colonisation of urogenital or anorectal sites have been reported, mainly in females.
Diagnostic considerations: Co-infections
In patients who present with urethritis or other symptoms suspicious for a sexually transmitted infection, it is important to consider co-infections with other STIs. 15 to 19% of men may have a concurrent infection with Chlamydia trachomatis (CT). It is therefore important to test for both chlamydia and gonorrhea by nucleic acid tests (NATs). Either a first-void urine or urethral swab is suitable for these tests. In addition, a further swab for bacterial culture should be ordered.
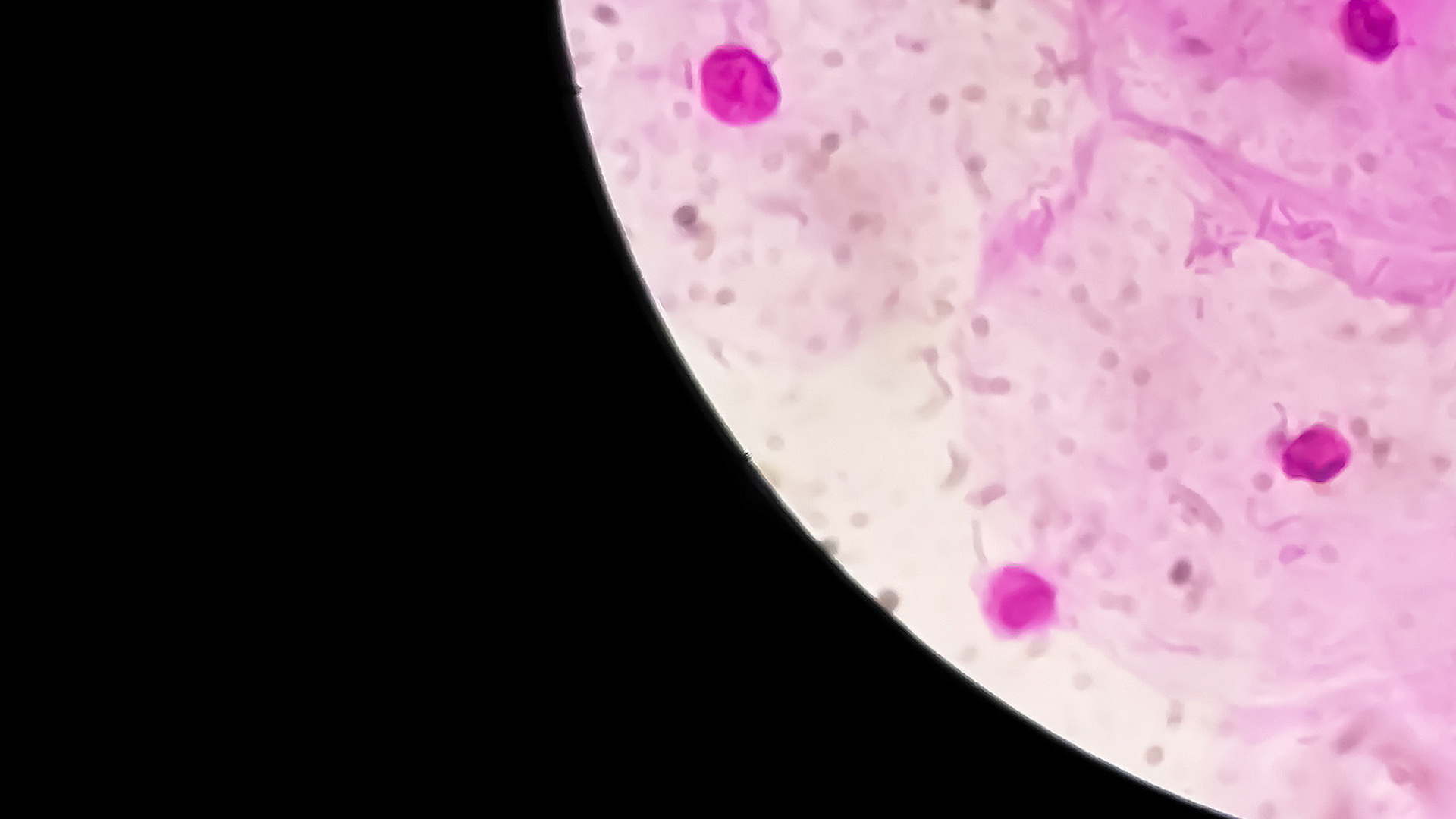
Laboratory diagnosis of meningococcal anogenital infection
Gram stain is routinely performed on all genital swabs. The presence of Gram-negative cocci on the gram stain, and increased numbers of leucocytes, predominantly neutrophils, is suggestive of urethritis but cannot distinguish between NG and NM.
Bacterial culture is, therefore, the mainstay of diagnosis. Depending on the site of infection, collection of a urethral, genital, or anorectal swab for bacterial culture is required.
NM will not be detected by routine STI screening if only nucleic acid amplification tests (NATs) are used, but testing should be performed to rule out other infections. Dual infections with both Neisseria meningitidis and Neissseria gonorrheae can also occur, and previous infections with NG are common in MSM.
PCR testing of NG and CT without bacterial culture could lead to a missed diagnosis as the PCR can only detect Neisseria gonorrhoeae; it will not detect Neisseria meningitidis. Currently, there is no TGA-authorised PCR test available for the detection of meningococcal urethritis or anogenital infection.
There have been over 30 cases of NM at a urogenital or anorectal site reported in NSW since September 2023, and it is likely that many have gone undetected. The importance of actively testing, detecting, and treating cannot be overemphasised.
Mycoplasma genitalium: An Emerging Concern
Dr Linda Dreyer
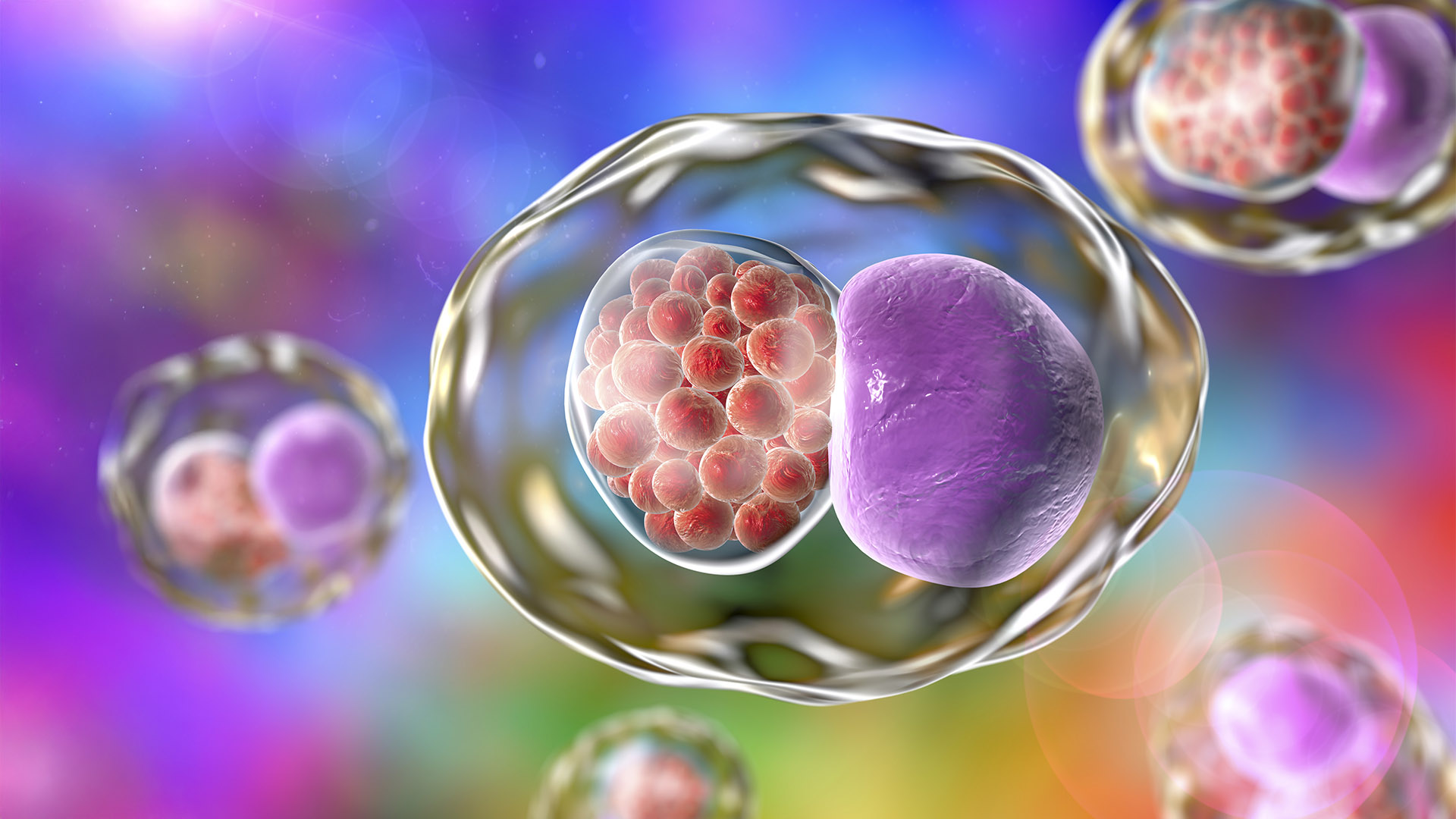
Mycoplasma genitalium is a bacterium that causes nongonococcal urethritis (NGU) in men and disease in the lower and upper reproductive tract of women.
Prevalence and risk factors
The prevalence of Mycoplasma genitalium in young adults (18-27 years old) is estimated to be approximately 1%, but is as high as 15-25% in men with symptomatic NGU and up to 15% of women with pelvic inflammatory disease (PID). In Melbourne, asymptomatic infection was detected in 9.5% of men who have sex with men (MSM). Rectal positivity was higher than urine (7.0% vs. 2.7%), and co-infection with other STIs was found in 17%.
Collection recommendations for accurate diagnosis
Mycoplasma genitalium presents with clinical symptoms and signs very similar to other STIs like chlamydia and gonorrhoea, which may complicate its diagnosis. Nucleic acid amplification tests (NAATs) are the recommended diagnostic method, offering high sensitivity and specificity. The best sample to obtain is a first-pass urine sample in male patients or a high vaginal swab in female patients. A cervical swab is slightly less sensitive, with a first-pass urine sample being the least sensitive in female patients. In high-risk populations, a rectal swab should also be collected. As pharyngeal infection is uncommon, a throat swab is not indicated.
The growing challenge of antibiotic resistance
The primary concern in treating Mycoplasma genitalium is its increasing resistance to antibiotics. Azithromycin (macrolide) resistance is widespread, prompting a shift towards alternative regimens like moxifloxacin. However, resistance to moxifloxacin is also emerging, creating a significant challenge in management. In Australia, the current resistance rate of azithromycin exceeds 60% in the majority of cases and is even as high as 80% in the MSM population.
Treatment is based on the test results and clinical presentation. See STI guidelines.
A doctor’s role in prevention
Preventive measures are crucial in managing Mycoplasma genitalium. Regular STI screening, safe sex practices, and public health campaigns can significantly mitigate its spread. It is vital for doctors to counsel patients on safe sex practices and the importance of regular screening. However, the significance of M. genitalium in asymptomatic individuals remains uncertain. Currently, local guidelines advise against testing asymptomatic patients unless they were exposed to known contact.
Managing the Mycoplasma genitalium challenge
Mycoplasma genitalium represents a significant and growing challenge in sexual health. The evolving nature of its antibiotic resistance profile necessitates a vigilant approach to diagnosis, treatment, and public health strategies. Continuous education and updated guidelines are essential to effectively manage this emerging STI.
The Changing Landscape of STIs: A GP’s perspective
By Dr David Baker

Dr David Baker, a GP and Director of East Sydney Doctors, has worked in Darlinghurst for over twenty years. He has a special interest in Sexual Health and HIV Medicine and has completed additional training at The University of Sydney – obtaining a Diploma in Medicine (Sexual Health).
As we have all seen over the last few years, we need to expect the unexpected in health care. This remains true in the world of Sexually Transmitted Infections (STIs), as we saw with the rise and fall of monkeypox (now renamed mpox).
Some things don’t change. GPs continue to play a vital role in the prevention, diagnosis, and treatment of STIs. Getting to know our patients is very important, especially when it comes to screening for STIs. With a new patient, we can ask about their background in terms of sexual behaviour, relationship status, and risk factors such as travel history. STI testing will depend on the clinical situation as well as the patient’s background.
Testing guidelines: asymptomatic patients
Current guidelines recommend
testing for asymptomatic patients to include first-catch urine for chlamydia and gonorrhea PCR
testing, along with a blood test for HIV antigen/antibody, syphilis serology, and hepatitis B
serology (HBsAg, anti-HBs, anti-HBc).9 Patients should be vaccinated for hepatitis B if
not immune.
Additional guidelines: MSM
Men who have sex with men (MSM) are recommended to
also have anal and rectal swabs for chlamydia and gonorrhea PCR testing, to undergo sexual health
screenings every 3 months, and to receive an annual hepatitis C antibody test (hepatitis C is rarely
an STI but can be transmitted in MSM).
HIV cases decline thanks to PrEP
HIV infections in Australia have markedly
declined to 552 HIV notifications in 2021, a 48% decline since 2012.10 Increasingly,
infections are occurring in females and people born overseas. HIV rates have fallen in the MSM
population largely due to the increased use of Preexposure Prophylaxis (PrEP) – antiretroviral
medications taken prior to sex. All MSM should be encouraged to use PrEP. Even though HIV rates are
falling, it is very important to continue regular HIV testing, as HIV is now manageable with modern
treatment but has a much better outcome if diagnosed early.
Rise in syphilis: Be aware of generalised rashes
Syphilis rates have greatly
increased over the last 10 years, particularly in MSM populations as well as in Aboriginal and
Torres Strait Islander people. Syphilis has been called the ‘Great Mimic’ as it causes a wide range
of symptoms. Primary syphilis is a painless ulcer at the site of infection but is often missed.
Secondary syphilis occurs 6 weeks or so later with a wide range of symptoms, particularly a rash.
Tertiary syphilis occurs usually years later and involves many organ systems. Most patients are
diagnosed by serology. An important take-home message is to order syphilis serology for any
generalised rash. Treatment is usually with intramuscular penicillin.
Drug resistance amidst the rise in gonorrhoea cases
Gonorrhoea rates have
also increased. Multidrug-resistant gonorrhoea is emerging around the world and has been reported in
Australia. It is important to follow treatment guidelines and, if possible, obtain a sample for
resistance testing.9
Order mycoplasma genitalium for symptomatic patients
Mycoplasma genitalium is
an uncommon cause of urethritis and cervicitis. Order this test if patients are symptomatic (e.g.,
urethral discharge) but not as a screening test. A swab or first-catch urine PCR test should be
collected. Treatment is complex and is guided by sensitivity testing.
Mpox prevention through vaccination
This infection is largely in the MSM
population, with exposure mostly occurring while travelling. The usual symptoms are lesions or
ulcers around the body. If suspected, a swab for PCR should be taken, and the laboratory notified.
Case numbers have dropped, with only 26 cases in Australia in 2023, making this a rare STI.11
Note: Mpox can now be prevented by vaccination.
Genital wart cases declining thanks to HPV vaccination
A good news story is
that genital wart infections are on the decline, thanks to universal HPV vaccination.
Important Updates from STI Guideline Changes 2020-2022
For more information, please visit sti.guidelines.org.au/whats-new.
- Standard asymptomatic check-up: HIV and syphilis testing should be included whenever STI testing is indicated.
- Chlamydia: To improve antibiotic stewardship, immediate treatment is not recommended for all sexual contacts of chlamydia – instead, offer testing of exposed anatomical sites and await results.
- Sex-associated diarrhoea: Among reports of increasing drug-resistant shigellosis among MSM, there is a need for expert local advice and stool culture when treating diarrhoea in MSM.
- Skin rash and lesions: Primary care clinicians are encouraged to think about STIs when examining, testing and managing clients with rashes, lumps and lesions that might not be on the genital skin.
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
How to Order STI Testing for Asymptomatic Patients
Complete the Clinical Labs general pathology request form, listing the recommended STIs for asymptomatic screening: Gonorrhoea, chlamydia, syphilis, HIV, Hepatitis B and Hepatitis C.
In the Clinical Notes, add “STI Screen”.
Urethral swabs, first-pass urine (FPU) and vaginal/endocervical swabs. Note: Vaginal/endocervical swabs are more sensitive than FPU samples in female patients.
Serology for HIV, syphilis, Hepatitis B and Hepatitis C.
Bulk-billed, subject to Medicare eligibility criteria.
References
-
Sexually Transmitted Infections (STIs) (2023). World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/sexually-transmittedinfections-(stis) (Accessed: 07 February 2024).
-
Dashboard · NINDSS Portal. Available at: https://nindss.health.gov.au/pbi-dashboard/ (Accessed: 02 February 2024).
-
McDonald, R. et al. (2023) ‘Vital Signs: Missed Opportunities for Preventing Congenital Syphilis — United States, 2022’, MMWR. Morbidity and Mortality Weekly Report, 72(46), pp. 1269–1274. doi:10.15585/mmwr.mm7246e1
-
Multi-drug Resistant Gonorrhoea (2023). World Health Organization. Available at: https://www.who.int/news-room/fact-sheets/detail/multi-drug-resistantgonorrhoea (Accessed: 08 February 2024).
-
Dionne-Odom, J. et al. (2022) ‘Coinfection with Chlamydial and Gonorrheal Infection among US Adults with Early Syphilis’, Sexually Transmitted Diseases, 49(8). doi:10.1097/olq.0000000000001605.
-
Burns BL, Rhoads DD. Meningococcal urethritis: Old and new. 2022. J Clin Microbiol. 60:6-8.
-
Toh E, Gangaiah D, Batteiger BB et al. Neisseria meningitidis ST11 Complex Isolates Associated with Nongonococcal Urethritis, Indiana, USA, 2015–2016. 2017. Emerg Infect Dis. 23(2): 336-339.
-
Nickmans S, De Beenhouwer MD, Vernelen K et al. Is Neisseria meningitidis a new cause of sexually transmitted disease? 2014. Clin Microbiol Newsletter. 36:1.
-
Australian STI Management Guidelines For Use In Primary Care. https://sti.guidelines.org.au/
-
HIV, viral hepatitis and sexually transmissible infections in Australia Annual surveillance report 2022. https://www.kirby.unsw.edu.au/sites/default/files/documents/Annual-Surveillance-Report-2022_HIV.pdf
Peel J., Bradshaw C. (2020). Medicine Today, 21(3):41-43.
Waites K.B., et al. (2023). Latest Advances in Laboratory Detection of Mycoplasma genitalium. Journal of Clin Micro, 61(3), e00790-21.
Manhart, L.E., Jensen, J. S. (2020). Mycoplasma genitalium: a review of current diagnosis and treatment. Infectious Disease Clinics, 34(2), 273-285.
Getman, D., Jiang, A., O’Donnell, M., & Cohen, S. (2019). Mycoplasma genitalium: An Overlooked Sexually Transmitted Pathogen in Women? Infectious Diseases in Obstetrics and Gynecology.
Taylor-Robinson, D., Jensen, J. S. (2011). Mycoplasma genitalium: from chrysalis to multicolored butterfly. Clinical Microbiology Reviews, 24(3), 498-514.
Bradshaw, C. S., & Fairley, C. K. (2019). Rapid point-of-care testing for sexually transmitted infections. The Lancet Infectious Diseases, 19(6), 570-578.
Stewart J., D., et al. (2020). Should we routinely test for Mycoplasma genitalium when testing for other sexually transmitted infections? Med J Aust, 212 (1): 30-31.
https://sti.guidelines.org.au/sexually-transmissible-infections/mycoplasma-genitalium/