New research supports STI reclassification and partner treatment
By Dr Linda Dreyer
Published September 2025
Bacterial vaginosis (BV) is the most common cause of abnormal vaginal discharge in women of reproductive age, affecting nearly 30% of women globally.1 It is characterised by a shift in the vaginal microbiota from protective lactobacillus dominance to an overgrowth of anaerobic bacteria such as Gardnerella vaginalis, Atopobium vaginae and Mobiluncus spp.1 This dysbiosis is associated with increased vaginal pH, amine production and a characteristic malodour.
Despite its prevalence, BV remains underdiagnosed and undertreated, particularly in asymptomatic cases. It is associated with significant reproductive health complications and an increased risk of acquiring sexually transmitted infections (STIs), including chlamydia, gonorrhoea and HIV.1 This update provides an overview of BV’s pathophysiology, diagnosis, treatment and new insights into partner management.
Clinical presentation
While many women with BV are asymptomatic, typical symptoms include a thin, white or greyish discharge with a distinct fishy odour. BV is more commonly detected among users of intrauterine devices (IUDs) and is associated with an increased risk of obstetric complications such as spontaneous abortion, preterm birth, chorioamnionitis and postpartum endometritis.1
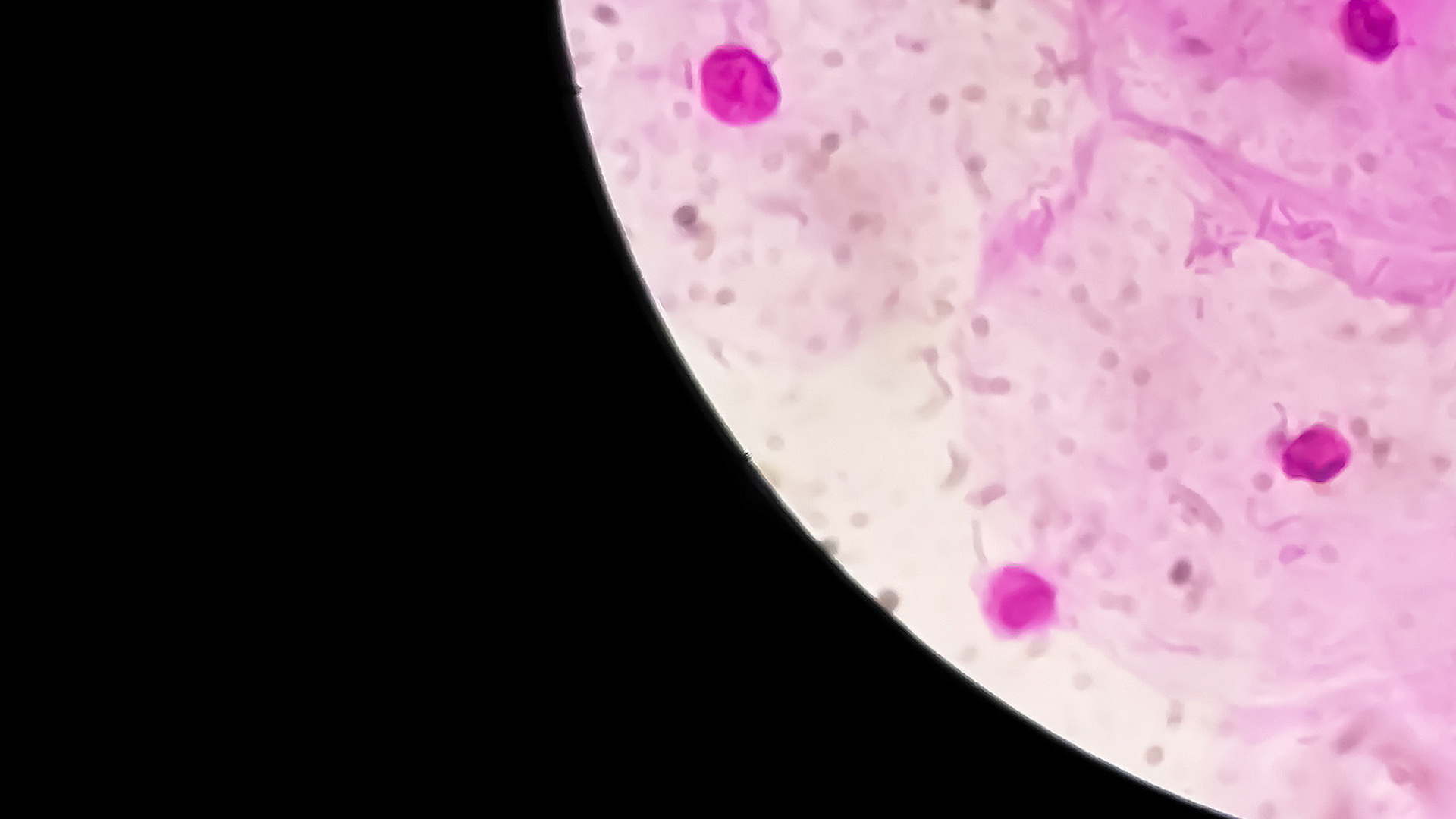
Diagnosis
Diagnosis of BV relies on either Amsel’s criteria or Nugent scoring from vaginal swabs. Amsel’s criteria require at least three of the following four features: homogeneous discharge, vaginal pH ≥ 4.5, clue cells on microscopy and a positive amine (“whiff”) test. Nugent scoring is based on Gram stain, with a score of 7–10 diagnostic for BV.1 Molecular diagnostic methods such as nucleic acid amplification tests (NAATs) can also detect BV-associated bacteria.
Management
First-line treatment
For non-pregnant women:
- Metronidazole 400 mg PO twice daily for 7 days (PBS listed)
- Clindamycin 2% intravaginal cream, 5 g nightly for 7 nights (not PBS listed)
- Metronidazole 0.75% gel, 5 g intravaginally nightly for 5 nights (not PBS listed)1
Patients should be advised to avoid alcohol during and for 48 hours after metronidazole treatment. Sexual contact should preferably be avoided. Condoms may be used if needed but as intravaginal creams may weaken latex condoms, barrier protection should be used cautiously.
For pregnant women, the same regimens apply. Metronidazole has not been associated with teratogenicity, and clindamycin is safe in pregnancy.1
Recurrent BV
Recurrence is common and occurs in over 50% of women within 3–12 months of treatment.2
Recommended management for recurrence includes:
- Metronidazole 0.75% gel, 5 g twice weekly for 4 months
- Consider specialist-guided use of intravaginal boric acid (compounded)1
Emerging evidence suggests that recurrence is often driven by reinfection from untreated partners.2
Partner Treatment: A paradigm shift
Due to lack of efficacy, treatment of male partners was not recommended historically. However, a 2025 randomised controlled trial (RCT) led by Vodstrcil et al. found that concurrent treatment of male partners significantly reduces recurrence of BV in women.3
In the trial, recurrence within 12 weeks occurred in only 35% of women whose partners received treatment, compared to 63% in the control group.
Male partner treatment regimen:
- Metronidazole 400 mg PO twice daily for 7 days,
AND
- Clindamycin 2% cream, applied to the penis twice daily for 7 days1
Synchronised treatment of couples is advised. Both partners should abstain from sexual activity during treatment or use barrier methods if needed. Adverse effects in men were mild and included nausea, headache and a metallic taste.3
Women with female partners
High concordance of BV has been observed in women who have sex with women. Although no trials have yet confirmed the efficacy of partner treatment in this population, testing and synchronised treatment may reduce reinfection risk.1 A current trial (PACT study) is underway to assess efficacy in this community.
Recommendations for GPs
- Always treat symptomatic BV and offer treatment for asymptomatic women requesting care or undergoing invasive procedures.
- Educate patients about the role of sexual transmission and the importance of partner management.
- Consider offering partner treatment, especially in ongoing male-female relationships, in line with new evidence.
- Reinforce adherence, avoidance of intravaginal cleaning products, and consistent condom use.
- Refer complex or recurrent cases to sexual health specialists for further management, including adjunct therapies.
Conclusion
Emerging research has redefined BV as a sexually associated condition, challenging traditional treatment approaches. With recurrence rates historically high, incorporating partner treatment represents a promising strategy for reducing recurrence and improving long-term outcomes. GPs play a pivotal role in diagnosis, treatment and patient education to minimise the reproductive morbidity associated with this common condition.
Bacterial Vaginosis: Rethinking management with partner treatment
By Dr Binay Kumar

Dr Binay Kumar is a GP and Director at Lilydale & Mt Evelyn Doctors in Melbourne’s outer east. He has a special interest in cosmetic medicine and preventative care, with clinical experience across India, the UK and Australia.
Bacterial vaginosis (BV) is a common presentation in general practice, caused by an imbalance in the vaginal microbiome. It typically presents with a thin, grey discharge and a characteristic fishy odour, though some women remain asymptomatic.
Diagnosis is usually clinical, and first-line therapy remains oral metronidazole or intravaginal clindamycin. However, recurrence is common; over half of women relapse within three to six months. Traditionally, management has focused only on the woman, with little evidence supporting treatment of sexual partners.
A landmark 2025 NEJM trial from Australia demonstrated that treating male partners in heterosexual monogamous couples significantly reduced recurrence. Male partners were prescribed oral metronidazole (400 mg twice daily for seven days) plus topical clindamycin 2% cream applied to the penis twice daily. The trial was stopped early due to clear clinical benefits: recurrence fell from 63% to 35%, and adverse effects in men were mild and manageable.
These findings strongly support BV’s classification, at least in part, as a sexually transmitted infection. Reinfection from untreated partners appears to be a key driver of recurrence.
In my own practice, I have begun discussing partner treatment with women experiencing recurrent BV. When appropriate, I offer concurrent partner therapy, explaining the rationale. Most patients welcome this proactive, longer-term strategy.
While this approach may not be suitable for every case, it represents a valuable addition to our management toolkit. Importantly, local guidance is evolving: Melbourne Sexual Health Centre has already incorporated partner therapy into practice, endorsed by the RACGP.
As formal guideline revisions are awaited, we can consider a couple-focused approach in selected patients, potentially reducing recurrence, improving outcomes and shifting the way we think about BV.
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
How to Order Bacterial Vaginosis Testing
Complete the Clinical Labs general pathology request form, requesting vaginal/genital swab MCS.
Vaginal swab or genital swab.
Bulk-billed, subject to Medicare eligibility criteria.
References
-
Melbourne Sexual Health Centre. Bacterial Vaginosis Treatment Guidelines. 2024. Available from: https://www.mshc.org.au/.
-
Bradshaw CS, Vodstrcil LA, Hocking JS, et al. Recurrence of bacterial vaginosis is significantly associated with post-treatment sexual activity. Clin Infect Dis. 2013;56(6):777–786.
-
Vodstrcil LA, Plummer EL, Fairley CK, et al. Male-Partner Treatment to Prevent Recurrence of Bacterial Vaginosis. N Engl J Med. 2025;392(10):947–957. DOI: 10.1056/NEJMoa2405404.
-
Peebles K, Velloza J, Balkus JE, et al. High Global Burden and Costs of Bacterial Vaginosis. Sex Transm Dis. 2019;46(5):304–311.