Which tests to order for a timely diagnosis and to avoid complications
By Dr Wessel Jenner
Published December 2023
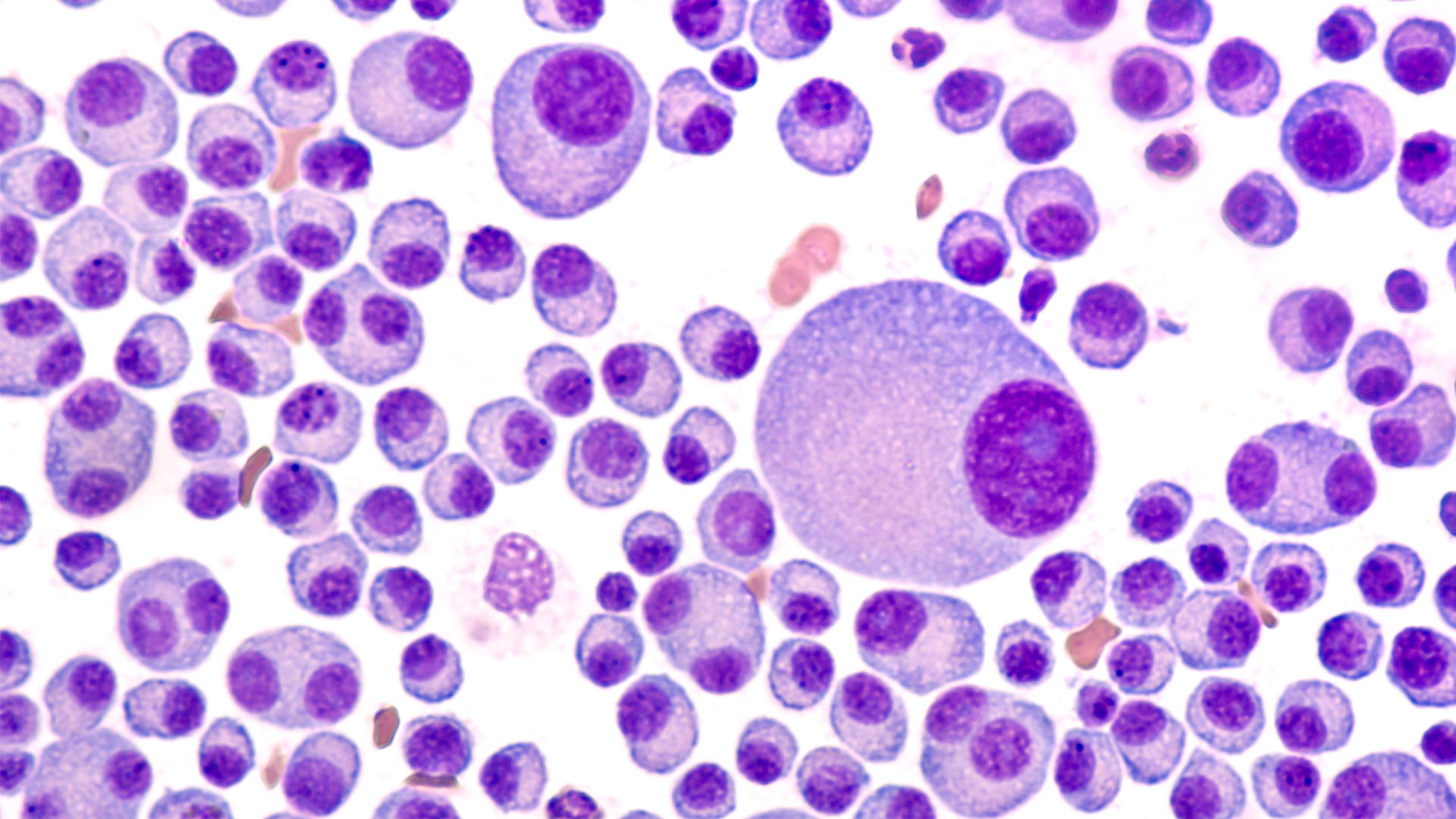
What is multiple myeloma?
Multiple myeloma is a blood cancer arising from plasma cells in the bone marrow. In Australia, it is estimated that 2,625 new cases of multiple myeloma were diagnosed in 2022, accounting for 1.6% of all new cancer cases diagnosed that year.1 The incidence rate for multiple myeloma increases with age and is highest for those aged 85–89 years1; however, it is also diagnosed in younger people.
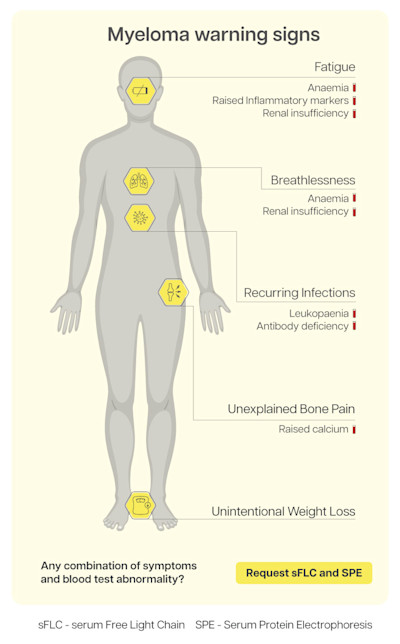
Signs and symptoms of multiple myeloma
Multiple myeloma symptoms are non-specific and may mimic the ageing process or more common conditions encountered in primary care, such as diabetes, hypertension and cardiac disease.2 Patients often present in primary care feeling generally unwell, with unexplained and persistent bone pain, back pain and body aches.2 As multiple myeloma progresses, advanced presentations are associated with end-organ damage. These are referred to as CRAB events of multiple myeloma and include:
- hyperCalcaemia,
- Renal impairment,
- Anaemia and
- Bone lesions.
Consequences of a delay in diagnosis and why a timely diagnosis is important
More than 50% of multiple myeloma patients experience a delay in diagnosis of over 6 months when diagnosed in primary care settings.3 Over 70% of patients experience additional symptoms and complications due to a delayed diagnosis, such as fractures, spinal cord compression, and renal failure.4 In particular, the number of patients experiencing renal disease is 2.6 times higher when the diagnosis is made after 6 months compared to when the diagnosis is made in under 3 months.3 Timely diagnosis and subsequent management of multiple myeloma avoids complications that impact patients’ quality of life. Earlier diagnosis and, therefore, the commencement of treatment have been shown to significantly improve 5-year survival rates of patients.5 Specifically, more than 8 in 10 (84%) myeloma patients will survive for more than 5 years when diagnosis is made early, compared with fewer than 3 in 10 (26%) when diagnosed at a later stage.5 It is also important to consider that if the patient develops too many complications, or the severity of the complications is too great, the haematologist may decide to limit patient treatment due to frailty. Primary care providers play a key role in recognising and ruling out multiple myeloma at the earlier stages of the disease.
Request correct blood tests to rule out multiple myeloma
A number of blood tests are recommended to rule out multiple myeloma, as highlighted in the publication by Dr Joseph Mikhael, MD, and Chief Medical Officer, International Myeloma Foundation. This includes, although not limited to, the following:2
- Complete Blood Count - to check for anaemia and raised Erythrocyte Sedimentation Rate (ESR).
- Serum Biochemistry Panel - to check for raised calcium, raised creatinine, and low albumin.
- Serum Protein Studies - to check for a monoclonal protein using serum free light chain (sFLC) and serum protein electrophoresis (EPG) tests.
The testing combination of sFLC + EPG has been shown to identify >99% of multiple myeloma patients.6
This is why current expert guidelines, such as those from the International Myeloma Working Group (IMWG)7 and the local ANZ Medical Scientific Advisory Group (MSAG) to Myeloma Australia, recommend this testing combination for initial screening and diagnosis of multiple myeloma.
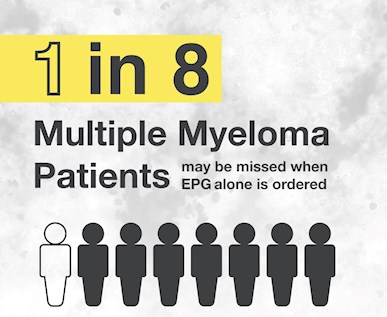
Significant deviation from these guidelines may cause diagnosis to be delayed or missed altogether due to the use of less sensitive testing panels. Data shows that 1 in 8 multiple myeloma patients may be missed when EPG alone is ordered.8
Refer to haematology
When the patient’s symptoms and basic laboratory findings are suggestive of multiple myeloma, an assessment of serum protein studies will help to rule out multiple myeloma.2 The survival rate for multiple myeloma patients increases by over 1.5 times when the diagnosis is achieved through the primary care referral pathway rather than the emergency route.9 Requesting the best test combination to rule out multiple myeloma earlier allows for a timelier referral pathway to haematology.
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
References
- Government A. Multiple myeloma in Australia statistics. 2022
- Mikhael J, et al. Multiple Myeloma for the Primary Care Provider: A Practical Review to Promote Earlier Diagnosis Among Diverse Populations. Am J Med 2023; 136:33-41
- Kariyawasan CC, et al. Multiple myeloma: causes and consequences of delay in diagnosis. QJM 2007; 100:635-640
- Europe MP. MYELOMA DIAGNOSIS ACROSS EUROPE. 2022; 1-56
- Bloodwise. The Current State of Blood Cancer Diagnosis in England. 2019; 1-22
- Katzmann JA. Screening panels for monoclonal gammopathies: time to change. Clin Biochem Rev 2009; 30:105-111
- Genzen JR, et al. Screening and Diagnosis of Monoclonal Gammopathies: An International Survey of Laboratory Practice. Arch Pathol Lab Med 2018; 142:507-515
- Katzmann JA, et al. Screening panels for detection of monoclonal gammopathies. Clin Chem 2009; 55:1517-1522
- Elliss-Brookes L, et al. Routes to diagnosis for cancer - determining the patient journey using multiple routine data sets. Br J Cancer 2012; 107:1220-6