A clinical guide to diagnosis and treatment
By Dr Phoebe Stanford
Published July 2025
Understanding Vitamin D: Function, sources and metabolism
Vitamin D is a fat-soluble vitamin which plays a key role in calcium and phosphate homeostasis and is important for bone and muscle function.
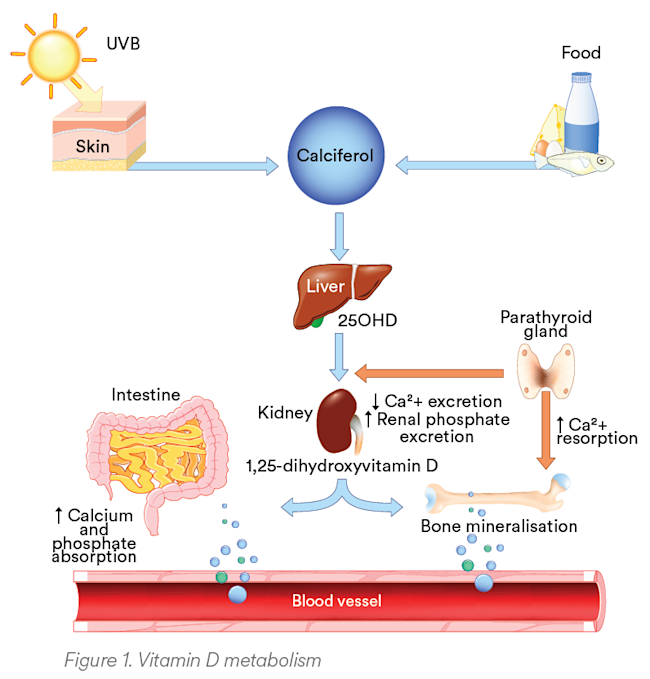
As there are few vitamin D-rich foods, skin production through the action of UV radiation is generally the main natural source of vitamin D. Vitamin D (calciferol) from the diet or supplements, or produced in the skin, requires conversion in the liver to the main circulating form, 25-hydroxyvitamin D (25OHD), which has a half-life of 2–3 weeks (see Figure 1). This is then converted in the kidneys to the biologically active form, 1,25-dihydroxyvitamin D, which has a half-life of just 4-6 hours.1
Certain medications (including some anticonvulsants) can increase the breakdown of vitamin D. Patients taking these medications are at increased risk for vitamin D deficiency and may require higher doses of vitamin D supplementation.
Vitamin D is taken up and stored in adipose tissue and may not be released unless there is fat breakdown, resulting in reduced circulating levels of 25OHD in obese individuals.
Recommended UV exposure for adequate vitamin D
The amount of sun exposure required for adequate endogenous vitamin D production depends on several factors, including time of the day/year, latitude, skin colour and the area of skin exposed. As a guide, to achieve adequate endogenous production of vitamin D, the following sun exposure times (in minutes per day) are recommended for individuals with moderately fair skin (based on exposure of hands, face and arms).2 For people with highly pigmented skin, the required exposure time would be 3–6 times longer.
| DECEMBER - JANUARY | JULY - AUGUST | |
|---|---|---|
| PERTH | 5-6 mins | 20-28 mins |
| ADELAIDE | 5-7 mins | 25-38 mins |
| MELBOURNE | 6-8 mins | 32-52 mins |
| HOBART | 7-9 mins | 40-47 mins |
| SYDNEY | 6-8 mins | 26-28 mins |
| BRISBANE | 6-7 mins | 5-19 mins |
| CAIRNS | 6-7 mins | 9-12 mins |
The required UV exposure for vitamin D synthesis needs to be balanced against the risk of skin cancer. For patients at very high risk of skin cancer, vitamin D supplements may be preferable to sun exposure as a source of vitamin D. Infants, the elderly in high care, indoor workers or those who cover their skin for various reasons also may not be able to achieve adequate sun exposure.
Clinical implications of vitamin D deficiency
Vitamin D deficiency results in reduced intestinal absorption of phosphate and calcium, which causes hypophosphataemia, hypocalcaemia and impaired mineralisation of bone. In addition, secondary hyperparathyroidism develops in response to the reduced calcium, promoting mobilisation of calcium from bone and phosphaturia, further exacerbating the bone mineralisation defect. With ongoing severe deficiency, this results in osteomalacia in adults and rickets in children.
Pregnancy
In pregnancy, maternal vitamin D deficiency not only places the mother at risk of accelerated bone loss, but also puts the baby at risk of rickets, hypocalcaemia/seizures and myopathy due to neonatal vitamin D deficiency.
Patients treated for osteoporosis
In addition to a negative effect on bone mineralisation, patients taking potent antiresorptive therapy are at risk of severe hypocalcaemia when these are used in the presence of vitamin D deficiency.
Eligibility for vitamin D testing
Vitamin D testing should be performed in those with risk factors for deficiency or in patients being investigated and/or treated for bone or mineral disorders. This is also required for funding by the Medicare Benefits Schedule (MBS).
Indications for vitamin D testing (MBS criteria):3
- Signs, symptoms and/or planned treatment of osteoporosis or osteomalacia
- Increased alkaline phosphatase with otherwise normal liver function tests
- Hyperparathyroidism, hypo- or hypercalcaemia, hypophosphataemia
- Malabsorption (e.g. cystic fibrosis, short bowel syndrome, inflammatory bowel disease, untreated coeliac disease, bariatric surgery)
- Deeply pigmented skin, or chronic and severe lack of sun exposure for cultural, medical, occupational or residential reasons
- Medications known to decrease 25OHD levels (e.g. anticonvulsants)
- Chronic renal failure and renal transplant recipients
And in children:
- Signs, symptoms and/or planned treatment of rickets
- Infants of mothers with established vitamin D deficiency
- Exclusively breastfed babies in combination with at least one other risk factor
- Siblings of infants or children with vitamin D deficiency
Measurement of vitamin D is not recommended as a screening test in the general population (including pregnant women and infants or children without risk factors).
Interpreting vitamin D test results
25OHD, the main circulating form of vitamin D, is the analyte routinely measured to assess vitamin D status. While there is no consensus on the optimal concentration of 25OHD, Australian guidelines recommend a target threshold of 50 nmol/L (60-70 nmol/l at the end of summer to allow for seasonal decrease) as adequate for mineral homeostasis, bone health and muscle function.5
Most laboratories in Australia, including Australian Clinical Labs, measure vitamin D by automated immunoassay. While there are differences in analytical precision between assays, a difference of ± 20% for repeated tests on the same sample is considered acceptable measurement uncertainty.4 On this basis, together with the seasonable variability, results between 50–70 nmol/L may be considered borderline for sufficiency.
Excessive vitamin D supplementation may rarely cause toxicity, manifesting as hypercalcaemia and hypercalciuria. The 25OHD level at which hypercalcaemia occurs is not well defined. 25OHD concentrations greater than 250 nmol/l may be considered a risk for toxicity, although hypercalcaemia is not usually reported until concentrations exceed 500 nmol/l.5
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
Subscribe Today!
How to Order Vitamin D Testing
Note the reason for testing to meet Medicare eligibility criteria for bulk-billing in the ‘Clinical Notes’ section on a Clinical Labs General Pathology Request Form.
Blood samples can be collected at any Clinical Labs collection centre.
Due to the long half-life, repeat testing should not be performed earlier than 3 months after either starting or changing the dose of vitamin D supplements.
Serum calcium, phosphate and parathyroid hormone will assist in placing the vitamin D level within the context of overall calcium homeostasis.
If osteoporosis is present, assessment of bone turnover markers (fasting C-terminal telopeptide of type 1 collagen [CTX] and procollagen type 1 N propeptide [P1NP]) may be considered to provide a way of monitoring bone turnover in response to therapy.
References
- Pazirandeh S and Burns D. Overview of vitamin D. Uptodate, Updated Sep 08 2023. Accessed April 2025.
- Working Group of the Australian and New Zealand Bone and Mineral Society, Endocrine Society of Australia and Osteoporosis Australia. Vitamin D and adult bone health in Australia and New Zealand: a position statement. MJA 2005; 182: 281–28.
- Australian Government Medicare Benefits Schedule Online. Medicare Benefits Schedule Item 66833 [Accessed 5 April 2025].
- RCPA Position Statement: Use and Interpretation of Vitamin D testing. The Royal College of Pathologists of Australasia, May 2013.
- Vitamin D and health in adults in Australia and New Zealand: a position statement. MJA 196(11), 18 June 2012.