Overcoming barriers to healthcare and improving preventative health
By Associate Professor Chris Barnes
Published March 2025
Men in Australia face higher rates of preventable diseases, lower engagement with healthcare services and shorter life expectancy than women.1 Cardiovascular disease, type 2 diabetes and chronic kidney disease are among the leading causes of death in men, yet many of these conditions can be prevented or managed through routine health screening. Despite this, men are significantly less likely to visit their general practitioner (GP) for routine health checks, leading to late-stage diagnoses and poorer health outcomes.2
Blood tests present an under-utilised opportunity for GPs to engage men in healthcare, promote preventative health strategies and improve health literacy. Annual blood tests provide objective, actionable data that can motivate men to take an active role in their health, facilitating early intervention and ongoing medical follow-up.3
Understanding the barriers to healthcare for men
Men are less likely than women to access primary healthcare, contributing to higher rates of undiagnosed and unmanaged chronic conditions. Several key factors contribute to this disparity:4
- Time constraints and perceived inconvenience: Many men cite work obligations, lack of time, and difficulty scheduling appointments as reasons for avoiding medical visits.
- A culture of self-reliance and reluctance to seek help: Societal expectations around masculinity often discourage men from acknowledging health concerns, leading to delayed medical consultations.
- Lack of awareness about preventative health: Many men associate healthcare with treatment rather than prevention, resulting in missed opportunities for early intervention.
GPs play a critical role in reducing these barriers by offering accessible, convenient and tailored approaches to men’s health screening. Blood tests provide a clear and measurable entry point for engaging men, shifting the conversation from reactive treatment to proactive prevention.
Recommended blood tests for male patients
Blood tests are a key component of preventative healthcare for men, offering early detection of cardiovascular, metabolic, endocrine and renal conditions. Current Australian guidelines recommend routine screening for common risk factors, particularly for men over 40 or those with predisposing risk factors.
Cardiovascular and metabolic screening
- Lipid Profile (Non-Fasting Preferred): The Royal Australian College of General Practitioners (RACGP) and the National Heart Foundation recommend lipid screening for all men over 45 years (or over 35 years for Aboriginal and Torres Strait Islander men). Non-fasting lipid tests are now widely accepted, improving compliance by reducing the inconvenience of early-morning, fasting-required visits.5
- HbA1c or Fasting Blood Glucose: Type 2 diabetes remains underdiagnosed in men, with many cases detected at later stages. Annual screening is recommended for men with obesity, hypertension or a family history of diabetes.
Prostate and hormonal health
- Prostate-Specific Antigen (PSA): The RACGP advises shared decision-making regarding PSA testing for prostate cancer in men over 50 (or over 40 for those with a family history). While routine screening is not universally recommended, early detection in high-risk individuals can improve outcomes.6
- Testosterone Levels: Low testosterone can impact energy, libido, muscle mass and mental health. Testing is recommended in symptomatic men, with repeat morning testing before confirming a diagnosis. Routine testosterone screening is not recommended for asymptomatic men, as low levels are often related to underlying health conditions rather than true hypogonadism. Testing should be reserved for those with clear clinical symptoms.7
Liver and kidney function
- Liver Function Tests (LFTs): Alcohol consumption and non-alcoholic fatty liver disease (NAFLD) are significant concerns among Australian men. Routine LFTs should be considered for men with metabolic syndrome, excessive alcohol intake or long-term medication use.
- Renal Function Tests (eGFR, Creatinine, UACR): Chronic kidney disease (CKD) is often asymptomatic in early stages. Routine screening is recommended for men with diabetes, hypertension or a history of cardiovascular disease.
Haematological and general health screening
- Full Blood Count (FBC): Anaemia and blood disorders often go undiagnosed until symptoms become severe.
- Vitamin D and Iron Studies: Low vitamin D and iron deficiency are associated with fatigue, muscleweakness and cardiovascular risk. Testing is particularly relevant for men with low sun exposure, dietary restrictions or symptoms of deficiency.
How laboratory testing can improve men’s health engagement
Many men only visit a doctor when symptoms become severe, missing crucial opportunities for early intervention. Blood tests provide an objective, measurable starting point for discussions about long-term health risks, increasing the likelihood of continued engagement.3
Key benefits of laboratory testing for men’s health engagement:
- Providing clear, objective health data: Many men respond well to quantifiable results. Discussing lipid levels, blood sugar trends or kidney function changes can motivate lifestyle modifications and adherence to medical advice.
- Normalising preventative health screenings: Integrating blood tests into routine health checks makes preventative care a habit rather than an exception.
- Reinforcing the importance of follow-up care: Tracking cholesterol levels, diabetes markers, or liver function over time allows GPs to guide incremental, achievable health improvements.
- Overcoming access barriers: Offering blood tests in workplace health programs, community centres or telehealth-supported models can improve uptake among men who struggle with time constraints and appointment scheduling.
Conclusion: A shift towards proactive men’s healthcare
Routine blood tests should be positioned as an essential tool in preventative healthcare for men—not just for early disease detection but as an engagement strategy that fosters long-term health literacy and proactive care.
By incorporating accessible, targeted and structured screening programs, GPs can overcome traditional barriers to men’s healthcare participation, ensuring more men take ownership of their health before conditions progress. Blood tests are a simple yet powerful intervention that can shift the focus from reactive treatment to long-term disease prevention, ultimately improving health outcomes and longevity for Australian men.
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
Subscribe Today!
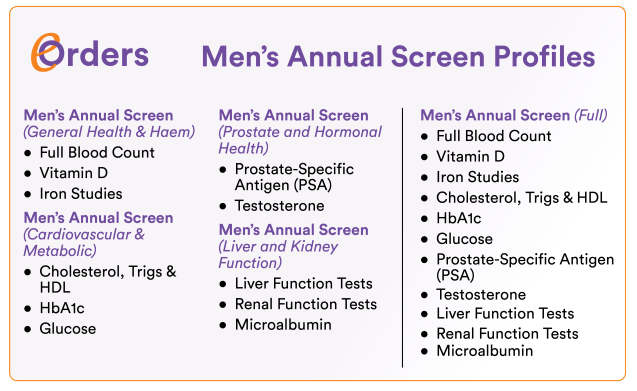
How to Order our ‘Men’s Annual Screen’ Profiles
For clinicians using eOrders in Best Practice, MedicalDirector Clinical or Clinical Labs eResults, we have developed a series of ‘Men’s Annual Screen’ profiles aligned with the clinical recommendations provided by A/Prof Barnes in this article.
Ensure eOrders with Clinical Labs is activated in your practice management software.
Navigate to ‘Clinical Recommendations’ (MD) or ‘Clinical Details’ (BP).
Select the desired ‘Men’s Annual Screen’ profile from the options described in the article
Bulk-billed, subject to Medicare eligibility criteria.
References
- Welfare, A.I.o.H.a., Deaths in Australia. 2024.
- Park, B. and Y.J. Lee, Upcoming Aging Society and Men’s Health: Focus on Clinical Implications of Exercise and Lifestyle Modification. World J Mens Health, 2020. 38(1): p. 24-31.
- Seidler, Z.E., et al., Approaches to Engaging Men During Primary Healthcare Encounters: A scoping review. Am J Mens Health, 2024. 18(2): p.15579883241241090.
- Macdonald, J.A., et al., Men’s and Boys’ Barriers to Health System Access. A Literature Review. 2022: Prepared for the Australian Government Department of Health and Aged Care, Canberra.
- Tse, T., et al., Non-fasting lipids: A change in practice. Australian Journal for General Practitioners, 2022. 51: p. 381-382.
- Rashid, P., K. Zargar-Shoshtari, and W. Ranasinghe, Prostate-specific antigen testing for prostate cancer: Time to reconsider the approach to screening. Australian Journal for General Practitioners, 2023. 52: p. 91-95.
- Grossmann, M., Androgen deficiency in older men. Australian Journal for General Practitioners, 2019. 48: p. 446-450.