The Urea Breath Test and Alternative Methods
By Dr Phoebe Stanford and Dr Stella Pendle
Published September 2024
Helicobacter pylori (H. pylori)
H. pylori is a Gram-negative bacillus that is found as a natural coloniser of the human gastric mucosa in about 50% of adults worldwide. H pylori was first identified in Australia by Marshall and Warren in 1983, who established the association with gastric and duodenal ulcers.1 More than 80% of duodenal ulcers and more than 60% of gastric ulcers (see Figure 1) are associated with H. pylori, as well as some cancers of the stomach.
Most infections are acquired during early childhood, postulated to be due to transmission from close family members by oral-oral or faecal-oral routes.2 In Australia, 25 to 30% of the population is infected, with the prevalence increasing with age. Acute infection may be asymptomatic or associated with mild dyspeptic symptoms. Acquisition of infection in adulthood is uncommon. Once acquired, the infection usually persists, resulting in chronic gastritis with the potential to cause gastroduodenal complications, including peptic ulcer disease, gastric atrophy, and intestinal metaplasia, as well as increasing the risk of gastric cancer and gastric mucosa-associated lymphoid tissue (MALT) lymphoma.
H. pylori may also be associated with iron and/or vitamin B12 deficiency due to reduced absorption caused by gastric atrophy and hypochlorhydria induced by chronic infection.
In adults, once H. pylori is diagnosed, eradication treatment is recommended.
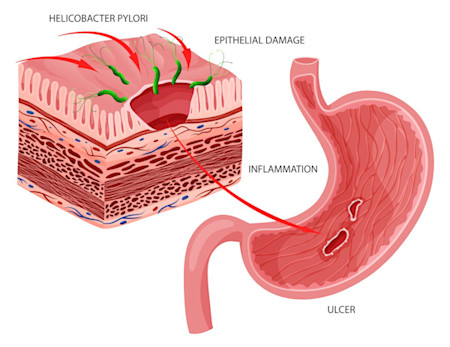
Figure 1. Gastric ulcer caused by H.pylori infection.
Diagnosis of H. pylori
The choice of test used to diagnose H. pylori is dependent on whether the patient requires an endoscopy to evaluate their symptoms. If an endoscopy is not required on the basis of clinical presentation, non-invasive tests for H. pylori are recommended.
Non-invasive tests are also useful where there is a potential false negative test during endoscopy (due to use of certain medications or active peptic ulcer bleeding) and for follow-up to confirm successful eradication after treatment.
Indications for testing (adults)3,4
- Established peptic ulcer disease
- Non-ulcer dyspepsia
- Monitoring the success of eradication of H. pylori after treatment
- Prior to chronic treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) or low-dose aspirin
- Unexplained iron deficiency anaemia (after investigation for other causes)
In children, testing is generally only recommended where there is established peptic ulcer disease or during endoscopy if treatment is intended. Such patients should be under specialist care.
Urea breath testing for H. pylori
The urea breath test is an accurate, non-invasive way to diagnose active H. pylori infection.
The test relies on the fact that H. pylori produces bacterial urease, which hydrolyses urea to produce CO2 and ammonia. This helps to neutralise gastric acid and allows H. pylori to survive in the gastric environment.
In the 14C Urea Breath Test, a capsule containing 14C-labelled urea is given by mouth, and 10 minutes later, exhaled breath is collected into a balloon. If H. pylori is present, 14CO2 will be produced, and this can be detected in the breath sample. If H. pylori is not present, the labelled urea will not be broken down, and the breath will not contain 14CO2.
Is the test safe?
14C is a naturally occurring radioactive form of carbon, present in very small amounts in all living things, with the more common form being 12C. The dose of radiation in the 14C Urea Breath Test is approximately equivalent to one day of background radiation exposure, far less than a standard X-ray.5
However, as studies have not been performed to determine safety in pregnancy, breastfeeding, and for children under 12 years, testing is not routinely performed in these groups. A stool antigen test is available as an alternative when testing for H. pylori is indicated.
Patient preparation
The patient will need to fast for a minimum of 6 hours before the test. The following medications should be discontinued before the test to prevent false negative results.
| Medication | Exclusion period |
|---|---|
| Antibiotics and bismuth containing products | 4 weeks |
| Sucralfate | 2 weeks |
| Proton Pump Inhibitors | 7 days |
| Antacids and H2 Antagonists | No exclusion period, other than during fasting and during the test |
Testing to confirm eradication following treatment should be performed at least 4 weeks following completion of treatment.
Alternative tests
Invasive tests
Invasive tests require upper endoscopy to obtain gastric tissue biopsies, which can be used for bacterial culture, susceptibility testing, and histopathology. The main limitation of these methods is their invasiveness and the ability to analyse only a small part of the gastric mucosa.6 These tests are of value in the management of recurrent infection and in patients who are failing therapy, where specialist consultation is required.
Non-invasive tests
In addition to the urea breath test, non-invasive tests include serology and stool antigen tests.
These tests provide high reliability in the detection of H. pylori due to their high
sensitivity and specificity (Table 1). However, all of these methods have limitations, and the
selection of test will depend on the clinical circumstances. Only the urea breath test and stool
antigen test identify active infection.
The Stool Antigen Test (SAT)
The Stool Antigen Test (SAT) is based on the direct
identification of H. pylori in stool samples. SAT is recommended for both the primary diagnosis
of H. pylori infection and for the monitoring of therapy effectiveness. The test is
non-invasive, quick, and easy to use, with a sensitivity of 95% and specificity of 97%. It is suitable
for the diagnosis of H. pylori in children.
Serology
Antibodies to H. pylori appear in the blood 3 to 4 weeks
after infection and may be present for life. Serologic tests are widely available to diagnose
H. pylori. They are non-invasive, rapid, and can be used in screening populations. However,
there are a number of limitations. Serology may be positive due to the presence of an active infection
at the time of the test, a previous infection, or non-specific cross-reactive antibodies. The results
must therefore be interpreted within the context of the clinical illness. Antibodies do not decline
following treatment, so the test is of no value in monitoring therapy.
Table 1: Accuracy of H. pylori diagnostic methods6
| Specimen type | Sensitivity (%) | Specificity (%) |
|---|---|---|
| Non-invasive tests | ||
| Urea Breath Test | 96-100 | 93-100 |
| Stool Antigen Test | 95 | 97 |
| Serology | 76-84 | 79-80 |
| Invasive (requires Endoscopy) | ||
| Rapid Urease Test | 85-95 | 95-100 |
| Histology | 91-93 | 100 |
| Culture | 76-90 | 100 |
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
Subscribe Today!How to Order the 14C Urea Breath Test
Request ‘Urea Breath Test’ on a Clinical Labs General Pathology Request Form.
The Urea Breath Test is bulk-billed subject to Medicare criteria, which includes both confirmation of H. pylori colonisation and monitoring of successful eradication.
Testing to confirm eradication following treatment should be performed at least 4 weeks following completion of treatment.
The Stool Antigen Test (SAT) – Specify ‘Stool Antigen Test (SAT)’ on the request form.
Serology – Specify ‘Serology for H. pylori’ on the request form.
References
- Warren J, Marshall B. Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet 1983; 1:1273–75.
- Kusters J, van Vliet A, Kuipers E. Pathogenesis of Helicobacter pylori Infection. Clinical Microbiology Reviews 2006; 19(3): 449-490.
- Crowe S. Helicobacter pylori Infection. N Engl J Med 2019; 380:1158.
- Chey W, Leontiadis G, Howden C, Moss S. ACG Clinical Guideline: Treatment of Helicobacter pylori Infection. Am J Gastroenterol 2017; 112:212.
- Lamont T. Indications and diagnostic tests for Helicobacter pylori infection in adults (2023). UpToDate. Retrieved May 28 2024 from https://www.uptodate.com/contents/indications-and-diagnostic-tests-for-helicobacter-pylori-infection-in-adults
- Bordin, D.S.; Voynovan,I.N.; Andreev, D.N.; Maev, I.V .Current Helicobacter pylori Diagnostics. Diagnostics 2021, 11,1458. https://doi.org/10.3390/diagnostics11081458