A milestone for preventative medicine
By Associate Professor Mirette Saad
Published March 2024
On 1st November, 2023, Genetic Carrier Screening for cystic fibrosis (CF), spinal muscular atrophy (SMA), and fragile X syndrome (FXS) was added to the MBS, marking a significant milestone in accessible healthcare for all Australians. In the following article, we provide information on the covered conditions, outline the Medicare eligibility criteria, and share insights from several GPs on the transition to bulk-billing for this testing. This shift represents a significant advancement in preventative medicine within the domain of general practice, ultimately enhancing accessibility and affordability for patients.
Screening for CF, SMA, and FXS
Clinical Labs’ Genetic Carrier Screening test for CF, SMA, and FXS provides patients with information regarding their chances of having a child with any of these conditions.
- One in 20 people are carriers of at least one of these conditions;
- 90% of carriers have no family history;
- One in 160 couples will be found to be at risk of having an affected child.
Cystic fibrosis (CF)
- CF is a severe autosomal recessive genetic condition that causes lung and gastrointestinal problems
- Approximately 1 in 25 people are carriers of CF
- Clinical Labs’ CF screening covers more than 75 common mutations in the CFTR gene
- CF affects approximately 1 in 2,500 people
Spinal muscular atrophy (SMA)
- SMA is an autosomal recessive inherited neuromuscular disease historically associated with high morbidity and mortality
- Approximately 1 in 35 people are carriers of SMA
- Clinical Labs’ SMA screening identifies deletions of the SMN1 gene (one copy), which account for approximately 96% of the mutations in this gene
- SMA affects approximately 1 in 6,000 people
Fragile X syndrome (FXS)
- FXS, an X-linked condition, is the most common inherited form of intellectual disability
- Approximately 1 in 330 people are carriers of FXS
- FXS carrier screening is recommended for females, as it is inherited in a different way to CF and SMA. Female patients who have the gene change (number of CGG triplet repeats) in the FMR1 gene are found to be at risk of having a child affected by FXS, as the abnormal gene may expand over generations
- The size of these CGG triplet repeats determines the chance of the FXS gene failing to function in a normal way and, therefore, the clinical presentation
- Males can also carry the faulty FMR1 gene on their one X chromosome and may pass it on to their daughters. (Testing would incur a private fee - not eligible for Medicare billing)
- FXS affects approximately 1 in 3,600 men and 1 in 6,000 women
In addition to bulk-billed screening, Clinical Labs also offers expanded carrier screening options at an out-of-pocket cost for patients who want a broadened assessment of their risk of having a child with a genetic condition. For information about our Comprehensive and Ashkenazi Jewish Carrier Screening tests, click here.
Medicare Eligibility Criteria
Bulk-billed genetic carrier screening is now available to determine a couple’s combined risk of having a child with a genetic condition. Testing is available for all individuals, even those with no symptoms or family history. Male partners of the biologically female positive cases for CF or SMA (not FXS) are eligible for testing under Medicare cover. Please see below for specific Medicare criteria. Private fee may apply if criteria are not met.
New items 73451 and 73452
The patient who is planning pregnancy or already pregnant should be tested first under MBS item 73451 prior to testing the reproductive partner patient under MBS item 73452 to ensure an informative and clinically relevant test result is obtained in the relevant gene.
73451
Testing of a patient who is pregnant or planning pregnancy to identify carrier status for pathogenic or likely pathogenic variants in the following genes, for the purpose of determining reproductive risk of cystic fibrosis, spinal muscular atrophy, or fragile X syndrome:
a. CFTR;
b. SMN1;
c. FMR1.
One test per lifetime.
The intent of MBS item 73451 is to test an asymptomatic female chromosomal sex patient who is either planning a pregnancy or is already pregnant.
73452
Testing of the reproductive partner of a patient who has been found to be a carrier of a pathogenic or likely pathogenic variant in the CFTR or SMN1 gene identified by testing under item 73451, for the purpose of determining the couple’s reproductive risk of cystic fibrosis or spinal muscular atrophy.
One test per condition per lifetime.
The intent of MBS item 73452 is to test an asymptomatic male chromosomal sex patient who is the reproductive partner of the patient planning pregnancy or already pregnant and has been tested under item 73451.
Recommended by clinical guidelines
Genetic Carrier Screening should now be a routine part of pre and early pregnancy clinical management by GPs and specialists, with both RANZCOG1 and RACGP2 guidelines recommending that genetic carrier screening be offered to every woman and couple who are planning or in the first stage of pregnancy, regardless of their risk factors.
The importance of early screening
It is always recommended that testing is undertaken prior to pregnancy so that this vital information is known early, offering greater reproductive choices, such as:
- pre-implantation genetic diagnosis through IVF,
- using donor eggs (or donor sperm for CF and SMA),
- donor embryos, or
- adoption.
Early detection is paramount as it also allows more time for counselling.
For further information on how to order bulk-billed genetic carrier screening for CF, SMA and FXS, click here.
The Impact of Preventive Care in General Practice
By Dr Jung Yoon Huh
General practice holds a unique place in the healthcare system due to its focus on preventive care. It’s the very reason I chose this specialty and a sentiment shared by many of my colleagues. While it may not have the glamour of high-profile surgeries often depicted in medical shows, its significance runs deep.
I was thrilled when reproductive carrier screening became accessible through Medicare last November. This test targets two autosomal recessive disorders and one X-linked disorder: cystic fibrosis (CF), spinal muscular atrophy (SMA), and fragile X syndrome (FXS). The process is remarkably straightforward, a simple blood test with results delivered within weeks. If a woman is not a carrier, the journey ends there. However, if she is a carrier, the next step involves testing her current partner and providing genetic counselling as needed.
Although this can be conducted during pregnancy, a positive result can lead to more complex and
distressing implications. That’s why I seize every opportunity to introduce this screening test
during various consultations. Whether discussing contraception, STI screenings, routine vaccinations
for infants, or addressing concerns like heavy menstrual bleeding and iron deficiency, I broach the
topic. Recognising the time constraints many women face, juggling work and family, I provide written
materials and a request form, allowing them to choose the most convenient time for the test.
The
brilliance lies not only in the test’s accessibility and simplicity but also in its potential to
transform lives. For prospective parents, it offers a chance to prevent these conditions in their
children, an opportunity that is priceless and life-changing. In the realm of general practice,
prevention and education are as vital as treatment. So, let us continue our proactive journey,
championing health and well-being.

Dr Jung Yoon Huh
Medical Principal of The Madison Medical Practice, Northbridge, NSW
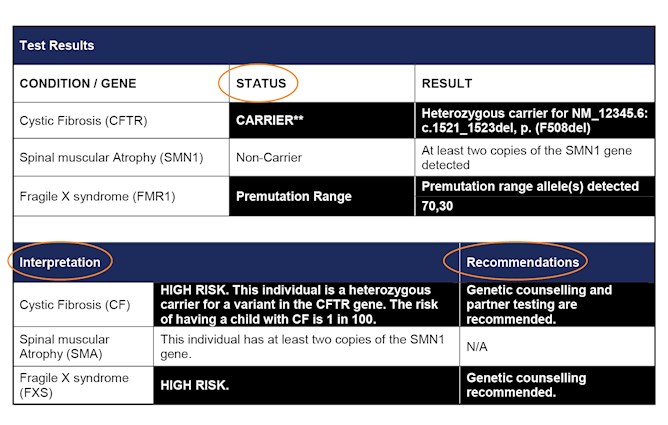
How to interpret test results
Status:
- Confirmation of patient’s carrier status for the tested condition (CARRIER/NON-CARRIER).
Interpretation:
- Patient’s risk of having a child with the specific genetic condition.
Recommendations:
- Pathologist’s advice on next steps regarding partner or follow-up testing/genetic counselling:
- If patient is found to be a CARRIER for CF or SMA → testing of reproductive partner is RECOMMENDED for that specific condition
- If patient is found to be a NON-CARRIER for CF or SMA → testing of reproductive partner is NOT REQUIRED
- If the reproductive partner is also found to be a CARRIER for CF or SMA → genetic counselling is RECOMMENDED (see below for details)
- If the patient is found to be in the pre-mutation or full mutation range for FXS → genetic counselling is RECOMMENDED (see below for details)
Figure 1. Extract from Clinical Labs Genetic Carrier Screening Report for CF, SMA, and FXS
Supporting you with genetic counselling for positive cases
For positive cases (tested by Clinical Labs), Clinical Labs offers one genetic counselling session per couple at no cost. Any follow-up consultations, if necessary, will incur an out-of-pocket fee.
- We will notify the referring clinician and provide contact details for the genetic counselling service.
- The referring doctor can either contact the genetic counsellor to schedule the appointment, or the consultation can be organised through the lab.
- Appointments are conducted over the phone and are generally available within 48 hours of referral.
During the call, which lasts 15-20 minutes, the genetic counsellor will discuss the risk of having a child carrying this condition with the patient and their partner. It is also optional for the referring clinician to be on the call.
Please note: The genetic counselling request must be made within two weeks of receiving the partner’s CARRIER test results. For FXS, only pre-mutation and full mutation cases are offered genetic counselling.
Supporting you through every stage of your patient’s pregnancy journey
In addition to genetic carrier screening, Clinical Labs also offers a wide range of routine and advanced antenatal pathology tests for patients, including our non-invasive prenatal test (NIPT), Harmony.
Australian clinical guidelines (RANZCOG3) recommend that doctors discuss NIPT with all pregnant women. Harmony NIPT screens for common foetal chromosomal abnormalities, including Down syndrome. It also evaluates foetal sex, sex chromosome aneuploidy conditions, and offers optional screening for 22q11.2 deletion (DiGeorge syndrome) at an additional cost to the patient. DiGeorge syndrome affects an estimated 1 in 1,000 pregnancies4,5 and is the second most common genetic cause of heart defects and developmental delay after Down syndrome.6
For more information about Harmony NIPT and other antenatal tests offered by Clinical Labs, click here.
The Role of Genetic Carrier Screening in Women’s Health Consultations
By Dr Sumudu Udapitiya
General Practitioner providing Shared Obstetric Care, Cranbourne West Medical Centre, VIC
I have been working as a GP in Australia since 2018 and am currently working at Cranbourne West Medical Centre in Victoria. My special interests include women’s health, and I also provide shared obstetric care for women. This places me in an ideal position to discuss preventive health and pregnancy planning with patients.
Having a healthy baby is the expectation of every woman planning a pregnancy. Genetic carrier screening, along with other general health assessments, plays a significant role in achieving this goal.
I have been offering pre-pregnancy genetic carrier screening from the start during all pregnancy planning consultations and have been discussing it opportunistically in women’s health consultations. I usually explain it with pictures to illustrate how genetic conditions are inherited and carried hidden among generations when the condition is autosomal recessive and X-linked. I also provide figures about carrier status to emphasise the importance of testing. Since there is no longer an out-of-pocket cost, I have seen a marked increase in acceptance for testing by most women.
As this is also a once-in-a-lifetime test, it gives the patient a sense of reassurance for future pregnancies if they are not a carrier or helps them plan for future pregnancies if they are a carrier. Testing in pre-pregnancy allows women to access genetic counselling in a timely manner and plan for a healthy baby.

Dr Sumudu Udapitiya
General Practitioner providing Shared Obstetric Care, Cranbourne West Medical Centre, VIC
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
References
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) Guidelines.
- The Royal Australian College of General Practitioners (RACGP) Guidelines.
- RANZCOG Guideline (C-Obs59) July 2018.
- Grati et al. Prenat Diagn 2015; 35: 801-809.
- Wapner et al. N Engl J Med 2012; 367: 2175-2184.
- Norton et al. N Engl J Med. 2015 Apr 23; 372 (17): 1589-97.





