Published July 2018
By Professor Sandra O'Toole
There has been a remarkable improvement in outcomes from breast cancer over the past 2 decades, with a 90% 5-year survival. Detection of earlier stage lesions through mammographic screening has played a role, as has the use of biologically targeted treatments such as tamoxifen and aromatase inhibitors for estrogen receptor (ER) positive cancers and HER2 targeted therapies in HER2 amplified breast cancers. Chemotherapy and radiotherapy have also reduced the risk of breast cancer recurrence and death. Multi-disciplinary care has contributed through better communication between members of the clinical team. However, patients and their treating doctors must make complex, personalised decisions and information from the pathology report plays a vital role in determining the type of treatment and prognosis for the patient.
This article will highlight the impact of key information from a pathology breast cancer report and will also update practitioners on the use of molecular prognostic tools such as Endopredict and Oncotype Dx to assist with adjuvant therapy decision making in ER positive breast cancer.
First diagnosis of early breast cancer
Breast cancer diagnosis is made through the “triple test” – correlating clinical and imaging features with a tissue pathology diagnosis. Fine needle aspiration can be used to confirm a diagnosis of malignancy but cytological preparations do not provide a reliable distinction between ductal carcinoma in situ (DCIS) and invasive carcinoma and also generally does not allow determination of hormone and Her2 receptor status. Increasingly, needle core biopsies are used to make the tissue diagnosis which allows preoperative assessment of tumour grade, type (invasive or DCIS, lobular or ductal invasive carcinoma) and receptor status, which assists with decisions about potential neoadjuvant chemotherapy as well as planning for surgery.
The definitive excision report
Detailed pathological assessment of the definitive excision specimen (whether a wide local excision or a mastectomy) provides a wealth of information on prognosis for the patient to guide further decisions about adjuvant therapy (chemo- and radiation therapy) or additional surgery. Pathology reports use a structured approach to ensure all key information is included but can be quite long. Some of the most important information is explained below:
Breast cancer type and grade
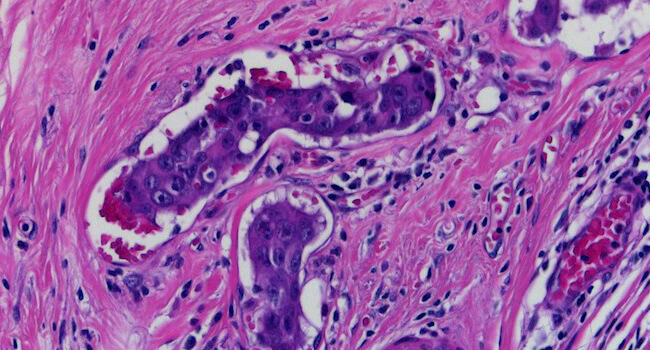
Invasive carcinoma is most commonly ductal carcinoma of no special type, with invasive lobular carcinoma the next most common. Invasive lobular carcinoma may show more extensive disease than appreciated clinically, or on imaging pre-operatively, and it is useful for this identification to assist with planning surgery. Tumour grade is a measure of tumour differentiation and is an important prognostic variable that influences decisions about additional treatment such as chemotherapy. Grading takes into account the ability of the tumour to make glands, the degree of nuclear pleomorphism and the proliferative rate measured by counting mitoses (Figure 1 – grade 1 invasive carcinoma, Figure 2 – grade 3 invasive carcinoma).
![This image depicts grade 1 invasive carcinoma. Professional medical imaging for clinical reference and educational purposes. [umbracoNodeId=9796]](/assets/image/jpeg/grade-1-invasive-carcinoma-388flzbxollwtxxzypol0i.jpg)
Figure 1: Grade 1 invasive carcinoma
![This image depicts grade 3 invasive carcinoma. Professional medical imaging for clinical reference and educational purposes. [umbracoNodeId=9798]](/assets/image/jpeg/grade-3-invasive-carcinoma-6f05id2oxges3xhbeoh5pv.jpg)
Figure 2: Grade 3 invasive carcinoma
Identification of invasive carcinoma within the blood vessels or lymphatics, lymphovascular invasion is an adverse prognostic finding and may influence the use of chemotherapy (See image at top of page).
Ductal carcinoma in situ (DCIS) is commonly seen in association with invasive carcinoma or alone. Detailed assessment of DCIS nuclear grade may also impact decisions regarding further surgery and/or radiotherapy. Descriptions of association with microcalcification (as commonly seen with necrosis in high grade DCIS) allow correlation with mammographic findings and may be helpful in monitoring patients by imaging in follow up.
Margins
Complete excision of both invasive carcinoma and DCIS is the goal of surgery and involved margins identified in the pathology report may prompt discussion in the clinical team and with the patient about the need for further surgery or radiotherapy.
Staging
In early breast cancer, this is primarily based on the size of the invasive carcinoma and the status of the associated axillary lymph nodes. For patients with clinically node negative disease, sentinel lymph node biopsies are often used to assess the nodal status. In some cases, often those patients with higher risk tumours, an intraoperative “frozen section” will be performed proceeding to axillary lymph node dissection in the same procedure if positive (Figure 3 –metastatic carcinoma in a lymph node). In others, the sentinel nodes will be assessed post-operatively with the definitive breast excision specimens. The most recent international staging system (AJCC 8th Edition) also incorporates grade, hormone and HER2 receptor status to assign a prognostic stage, highlighting the significant impact of targeted therapies on outcome.
![This image depicts metastatic carcinoma in a lymph node. Professional medical imaging for clinical reference and educational purposes. [umbracoNodeId=9800]](/assets/image/jpeg/metastatic-carcinoma-in-a-lymph-node-7ngijf4jevkkrsd5d5ejqj.jpg)
Figure 3: Metastatic carcinoma in a lymph node
Hormone and HER2 receptors
The hormone receptors for estrogen (ER) and progesterone (PR) are detected by immunohistochemistry in formalin fixed, paraffin embedded sections of invasive breast cancer and is a positive result in as little as 1% of tumour nuclei showing expression (Figure 4 – ER positive case). Proper handling of the specimen including optimal fixation is essential for reliable results. Around 80% of invasive carcinomas are ER positive with higher grade tumours less likely to be positive.
![This image depicts grade 3 invasive carcinoma. Professional medical imaging for clinical reference and educational purposes. [umbracoNodeId=9801]](/assets/image/jpeg/grade-3-invasive-carcinoma-7kibhy4bchbdpdmwxzwdz6.jpg)
Figure 4: Grade 3 invasive carcinoma
HER2 is assessed by immunohistochemistry (IHC) and by in situ hybridisation (ISH) where a DNA probe is used to directly label the HER2 gene and count the number of copies present. Around 15% of invasive breast carcinomas show amplification (extra copies) of the HER2 gene and these patients may receive HER2 targeted therapies such as trastuzumab. It has been estimated that the use of HER2 targeted therapies has resulted in a 50% reduction in death from this previously poor prognosis subtype of breast cancer. It is critically important to identify these patients so they receive the correct treatment, again highlighting the importance of optimal fixation and handling of breast cancer pathology specimens.
Molecular assays in breast cancer
Studies of gene expression conducted in the early 2000s highlighted the potential of molecular assays to provide additional information beyond traditional pathology about prognosis. A number of assays were developed including Oncotype Dx, Endopredict and the Prosigna assays among others. These assays have all been shown to provide useful prognostic information to ER positive patients about their risk of developing breast cancer recurrence and their use is supported by international guidelines. A recent large clinical trial using Oncotype Dx published in the New England Journal of Medicine (1) showed that women with ER positive, lymph node negative breast cancer over age 50 with low and intermediate scores had no difference in outcome when treated with endocrine therapy alone in comparison to the group who also received chemotherapy. This study highlights the clinical utility of molecular testing in sparing patients chemotherapy from which they are unlikely to derive significant benefit. Oncotype Dx is a first generation assay but a number of studies have shown that the second generation assays such as Endopredict (provided by Clinical Labs) which also incorporate clinical variables such as lymph node status and tumour size are better able to predict late recurrence (5-10 years post treatment) and may also identify a larger group of low risk patients (2,3). These assays are not currently funded by Medicare in Australia and are a significant out-of-pocket cost but are worth discussing with suitable patients given the potential benefits.
Summary
High quality pathology is a vital part of breast cancer diagnosis and management and molecular assays such as Endopredict can provide important additional information to support complex decision making about the use of chemotherapy in ER positive breast cancer.
References
- Adjuvant Chemotherapy Guided by a 21-Gene Expression Assay in Breast Cancer. Sparano JA, et al N Engl J Med. 2018 Jul 12;379(2):111-121.
- Comparison of EndoPredict and EPclin With Oncotype DX Recurrence Score for Prediction of Risk of Distant Recurrence After Endocrine Therapy. Buus R, et al J Natl Cancer Inst. 2016 Jul 10;108(11).
- Comparison of the Performance of 6 Prognostic Signatures for Estrogen Receptor-Positive Breast Cancer: A Secondary Analysis of a Randomized Clinical Trial. Sestak I, et al. JAMA Oncol. 2018 Apr 1;4(4):545-553.